What is Peripheral Vascular Disease? Symptoms and Causes Explained
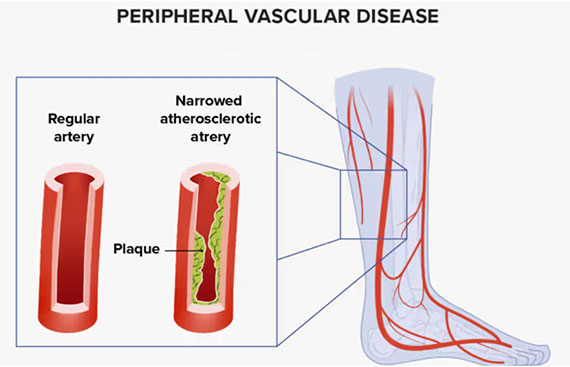
Peripheral Vascular Disease, PVD for short, is a circulatory condition involving blood vessels outside the heart and brain, mostly limbs, arms, and legs. PVD results from narrowing or blockage of blood vessels, which makes the flow of blood unsmooth inside the limbs.
In most cases, PVD often goes underdiagnosed because its symptoms are so mild. PVD, however, if left untreated may cause very severe complications. In this weblog, we're going to speak about what PVD is, commonplace signs, reasons, and a little of how some remedies like Trental 400 that has the content Pentoxifylline ought to help treat this ailment.
What is Peripheral Vascular Disease?
Commonly known as PVD, Peripheral Vascular Disease is also recognized through the medical term for Peripheral Artery Disease, or PAD. It is actually the boom of atherosclerosis that creates plagues, forms of buildup of fats in the lining of the arteries that narrow the blood vessels. Reduced oxygen supply from the blood flows to your limbs because of the narrowing or blockage of these blood vessels.
Even though PVD involves both arteries as well as veins, more people are affected whose artery is the one of their legs. If left continued in the long run it can cause tissue damage, ulcers, sometimes an amputation in lowered blood flow.
Peripheral Vascular Disease Causes
The most general symptoms of PVD are usually common and very slow in their onset, and often these symptoms only appear after the disease has progressed. The most common symptoms that commonly occur to people suffering from PVD are as follows:
- Painful Leg Cramping (Claudication): Claudication is the most not unusual symptom of PVD. Claudication refers to cramping, aching or ache inside the legs that often arise for the duration of bodily sports like walking or mountain climbing up the stairs. Pain will be relieved by way of resting. In this situation, your muscle mass within the legs don't get enough oxygen at the side of bodily interest.
- Numbness or Weakness: This is a revolutionary symptom of the ailment wherein you are laid low with numbness, weakness, or tingling sensation in your legs or feet. It occurs because the normal flow of blood towards the nerves decreases.
- Coldness in Lower Limbs: PVD can also come in the form of one leg feeling much colder than the other. The poor flow of blood to the affected limb makes it cold.
- Sores or Ulcers That Won't Heal. Poor flow of blood to the extremities could cause sores or ulcers, especially those lower extremities-the legs and feet. They won't heal or can be healing too slow.
- Discoloration: The skin would often become discolored typically on the lower extremities and it is due to low flow of blood. The general discoloration could be shiny or bluish in color due to reduced amount of oxygen supply to the tissue.
- Poor pulse in the legs: There will be weak or no pulse in the extremities due to poor flow of blood. This is direct sign of decreased flow of blood.
- Hair Loss on Legs: Due to the reduced blood flow, a person will eventually lose hair on legs or even up to the soles since the skin is not being adequately nourished and oxygenated.
- Impotence in Males: Some patients with PVD may additionally increase impotence because of the reality that the genitals are not receiving the desired blood glide.
If you are manifesting any of the signs and symptoms, see a physician for correct prognosis and remedy. In fact, the sooner Peripheral Vascular Disease is identified and its treatment started, the more limited it would have been, and the fewer complications it will have to take.
Risk Factors and Causes of Peripheral Vascular Disease
There are a number of chance elements and reasons related to Peripheral Vascular Disease:
- Atherosclerosis: This is the most common cause of PVD. In this disorder, the arteries are blocked due to plaque formation. Plaque consists of a mixture of fat and cholesterol, sometimes calcium, and other substances that are present in blood. This plaque collects inside the walls of arteries and thereby reduces the passage of blood through it.
- Most predisposing factors to PVD are smoking, which may damage blood vessels and increase the development of atherosclerosis. Therefore, the risk of developing PVD among those smoking is much higher than that of a non-smoker. Those suffering from diabetes are also liable to develop PVD due to the structural destruction of the blood vessels by hyper-glycemia and are easily subjects of narrowing and blockage.
- High Blood Pressure: It is chronic stress exerted to the arteries that supports the building of plaques and poses a risk for PVD.
- High Cholesterol, or Dyslipidemia: This state is characterised by elevated blood cholesterol levels, which could support the development of plaques in the arteries and lead to atherosclerosis and PVD.
- There is obesity, an excess weight and strains that weigh on the blood vessels and expose it more to the progress that develops into atherosclerosis, which eventually causes PVD.
- Age: PVD progresses with age, and most people who suffer from the condition are usually older than 50 years. Blood vessels become faulty with time and thus turn soft, and they easily fall into vulnerable spots into plaque formation.
- Poor circulation is one of the foremost causes of the development of PVD. This is due to a sedentary lifestyle.
PVD Treatment
The treatment of PVD addresses the control of its symptoms. This reduces chances of the progression of the disease. Treatment is mainly in the form of changing lifestyle and medicinal therapies in the form of medications. Surgery is not always a recourse.
1. Lifestyle Changes
- Smoking Abstinence: The best step to try to manage PVD is smoking cessation. Quitting smoking will slow down the disease progression process dramatically, hence enhancing blood flow .
- Balanced Diet: An consuming plan that lowers saturated fat consumption, ldl cholesterol, and sodium slows down the tempo at which plaque accumulates within the arteries.
- Exercise: Intensive exercise can increase blood flow to reduce signs of claudication. Walking, specifically, sporting events the muscle groups of the leg with a purpose to increase blood flow.
2. Medications
Many medications are given to the patient suffering from PVD. They could be:
- Blood Thinners: Aspirin or clopidogrel may be prescribed in order to avoid clotting in the narrowed arteries. Lipid Lowering Medications-Statins are prescribed to lower cholesterol levels and consequently plaque building.
- Trental 400 (Pentoxifylline): Trental 400 is the emblem call of a medication organized from Pentoxifylline. It is prescribed to patients suffering from PVD for improving blood flow. This is because it decreases the viscosity and hence thickness of the blood which allows easy flow in the narrower vessels. In addition to improving blood flow, Pentoxifylline may help alleviate the associated pain and cramping.
3. Surgery
In extreme cases, the procedures may have to be done surgically in reversing the flow of the blood. This may come in form of:
- Angioplasty and Stenting: Catheter has opened narrowed arteries with a small mesh tube called stent placed in location to keep the artery open.
- Bypass Surgery: Under this healing process, a wholesome blood vessel in the body that bypasses the blocked artery can be used to assist deliver blood circulate the affected limb.
Conclusion
Peripheral Vascular Disease is a serious disease and if not controlled can lead to quite grim complications. The symptoms are diagnosed earlier so that with the variation of lifestyle diseases would not aggravate further. Some drugs include Trental 400, which contains Pentoxifylline and may play a vital role in managing the symptoms and enhancing the flow of blood.
When you are a smoker, suffer from diabetes, or are exposed to other predisposing factors for PVD, you have to go to your health provider regularly for screenings and be compliant with recommended treatment. Proper management would do all the best and maximize quality of life while keeping the different risks associated with PVD at bay.
